
Major medical procedures such as surgery or chemotherapy are life-saving, but still highly damaging to the body's functions, causing a noticeable reduction in functional status after the procedure, followed by a recovery period that can last for years after discharge.
In recent years, increased focus has been placed on the concept of "prehabilitation" and improving the patient's baseline level of functional health and fitness prior to the medical procedure, so they will be better situated to recover afterwards.
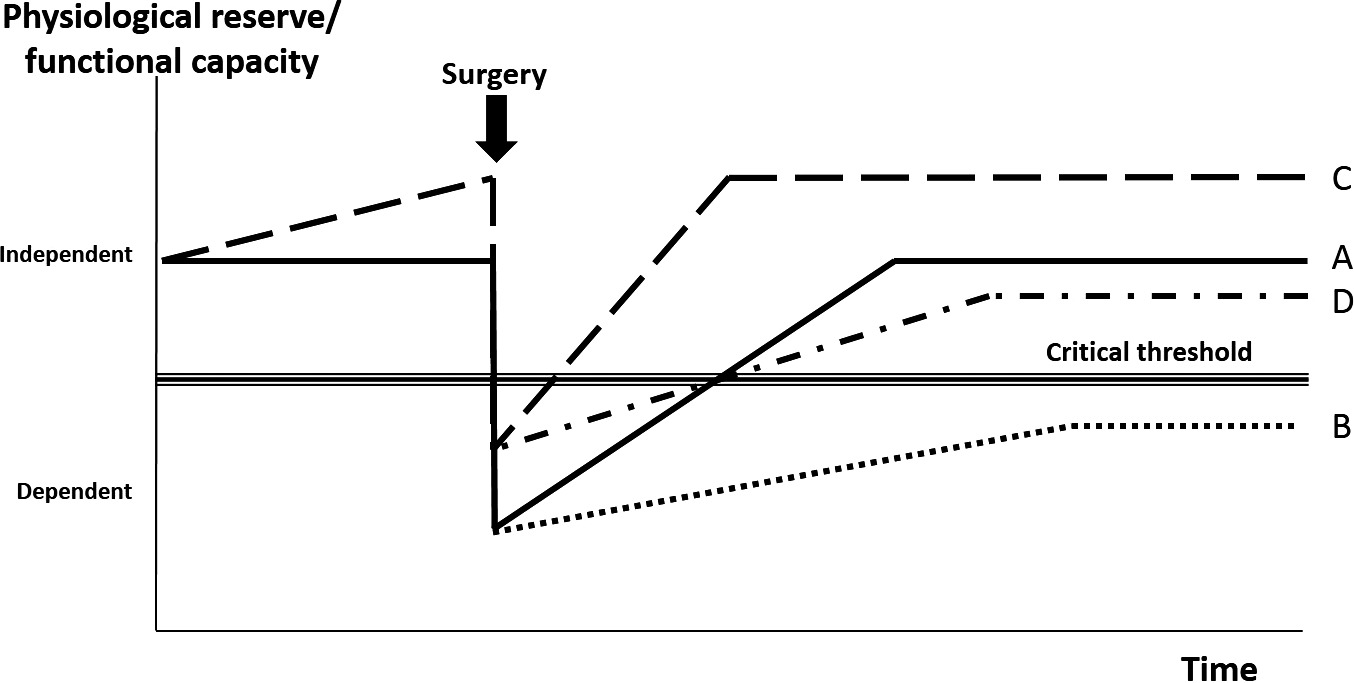
The chart above outlined in "Clinical guideline and recommendations on pre-operative exercise training in patients awaiting major non-cardiac surgery" (Anaesthesia 2018;73:750–68.) explains the prehabilitation concept in visual form! Following major medical intervention like surgery, a significant drop in physiological reserve/functional capacity occurs, followed by a recovery and rehabilitation phase (A). Those with a lower physiological reserve/functional capacity may be at an increased risk of peri-operative complications, which may also lead to slower or incomplete recoveries (B). Thus, prehabilitation is recommended, as this gives them higher physiological reserve/functional capacity before surgery, helping them recover more quickly and to a higher level (C). Even when there are complications, they are still better placed to retain better functionality and quality of life long-term (D).
How is prehabilitation conducted?
Typically speaking, prehabilitation programs are divided into 4 stages:
Screening (all patients)
Assessment (at-risk patients)
Intervention
Monitoring
Screening
This stage includes assessment of weight and body composition, how physically active/strong the patient is, harmful lifestyle habits such as smoking and alcohol, as well as psychological state and mental well-being. The goal is to find possible problems or weaknesses early on, and help the patient get as fit as possible prior to the procedure.
Assessment
Depending on the screening results, a further assessment may be useful to identify what specific training or adjustments are best for the patient's situation. For example, if physical activity screening indicates that a patient may have a poor fitness level (lack of regular exercise), a fitness assessment may be conducted, through methods such as grip strength assessment, 6 minute walk test, etc.
Typically, a body composition assessment may be included as well to determine the amount of muscle and fat in the body, and plan interventions that move both towards a healthier level. Overall, the assessment helps inform the prehabilitation team what the patient's needs are, how much support would be needed, and the best methods for improving overall physical, nutritional, and mental health within the limited time before medical procedure.
Intervention
This simply means the various actions taken to improve the patient's situation, whether it's quitting alcohol, beginning a fitness program, seeing a psychologist to mentally prepare, working with a dietitian to set and follow a healther diet, and other methods.
Monitoring
It's important to closely follow how effective prehabilitation activities are, to adjust as needed. Typically, the methods used during assessment may be used to help monitor progress, in addition to advice and encouragement as necessary.
The following table is an overview of common risk factor prehabilitation strategies:
| Risk factor | Screening | Assessment | Intervention | Prehabilitation goals |
| Physical activity | Inquire if patient regularly exercises sufficiently. Those that do not should be offered exercise prehabilitation | Physical fitness, including but not limited to cardio tests, walk tests, grip strength tests, etc. | Combined aerobic and resistance training program, based on results of objective fitness assessment | Improve aerobic capacity, build muscle |
| Inspiratory muscle training | Assess Respiratory Risk in Surgical Patients in Catalonia (ARISCAT) risk index score. Those with "intermediate" or "high-risk" should consider Inspiratory Muscle Training | Structured Inspiratory Muscle Training program | Develop respiratory muscles to reduce risk of pulmonary complications | |
| Smoking | Confirm if patient smokes, and if so, offer assistance to stop | Cessation program (ex: combination of counseling and nicotine replacement therapy) | Stop smoking before operation | |
| Alcohol | Confirm if patient drinks, and how much. Those with "hazardous" intake should undergo further assessment | Alcohol Use Disorders Identification Test (AUDIT) for those with higher intake | Alcohol intervention services | Reduce alcohol intake to non-hazardous levels |
| Nutrition | Malnutrition Universal Screening Tool (MUST) | Dietician/nutritionist assessment | Identify nutrient deficiencies, particularly protein following exercise training | Improve pre-procedure malnutrition, with diet that supports exercise training |
| Psychological factors | Hospital Anxiety and Depression Scale (HADS) | Poorly controlled depression, anxiety, and low self-confidence that might reduce engagement with prehabilitation | Build confidence, education programs, specialist input | Improve control of anxiety and depression, develop self-confidence to engage with prehabilitation and procedure |
To learn more, we recommend reading additional literature, such as this article published in Clinical Medicine (London), reviewing the evidence behind the concept of prehabilitation and the evidence of its impact, principles for developing prehabilitation in practice, and other practical implementation details.
Using the proper tools to conduct assessment and monitoring is important for evaluating how well a patient is progressing in their prehabilitation progress. Devices such as Grip Strength Dynamometers or Body Composition Analyzers are quick and easy-to-use methods that will provide practitioners with a good snapshot!